HeyDonto FHIR R4 API - Financial (1.0)
The Financial module covers the resources and services provided by FHIR to support the costing, financial transactions and billing which occur within a healthcare provider as well as the eligibility, enrollment, authorizations, claims and payments which occur between healthcare providers and insurers and the reporting and notification between insurers and subscribers and patients.
See also the Administration and WorkFlow modules.
Resources:
- Account - A financial tool for tracking value accrued for a particular purpose. In the healthcare field, used to track charges for a patient, cost centers, etc.
- Contract - Legally enforceable, formally recorded unilateral or bilateral directive i.e., a policy or agreement
- Coverage - Financial instrument which may be used to reimburse or pay for health care products and services. Includes both insurance and self-payment
- CoverageEligibilityRequest - Provides patient and insurance coverage information to an insurer for them to respond with information regarding whether the stated coverage is valid and in-force and optionally to provide the insurance details of the policy
- CoverageEligibilityResponse - Provides eligibility and plan details from the processing of an CoverageEligibilityRequest resource
- EnrollmentRequest - Provides the insurance enrollment details to the insurer regarding a specified coverage
- EnrollmentResponse - Provides enrollment and plan details from the processing of an EnrollmentRequest resource
- Claim - A provider issued list of professional services and products which have been provided, or are to be provided, to a patient which is sent to an insurer for reimbursement
- ClaimResponse - Provides the adjudication details from the processing of a Claim resource
- PaymentNotice - Provides the status of the payment for goods and services rendered, and the request and response resource references
- PaymentReconciliation - Provides the details including amount of a payment and allocates the payment items being paid
- ExplanationOfBenefit - Provides the claim details, adjudication details from the processing of a Claim, and optionally account balance information, for informing the subscriber of the benefits provided
- VisionPrescription - An authorization for the provision of glasses and/or contact lenses to a patient
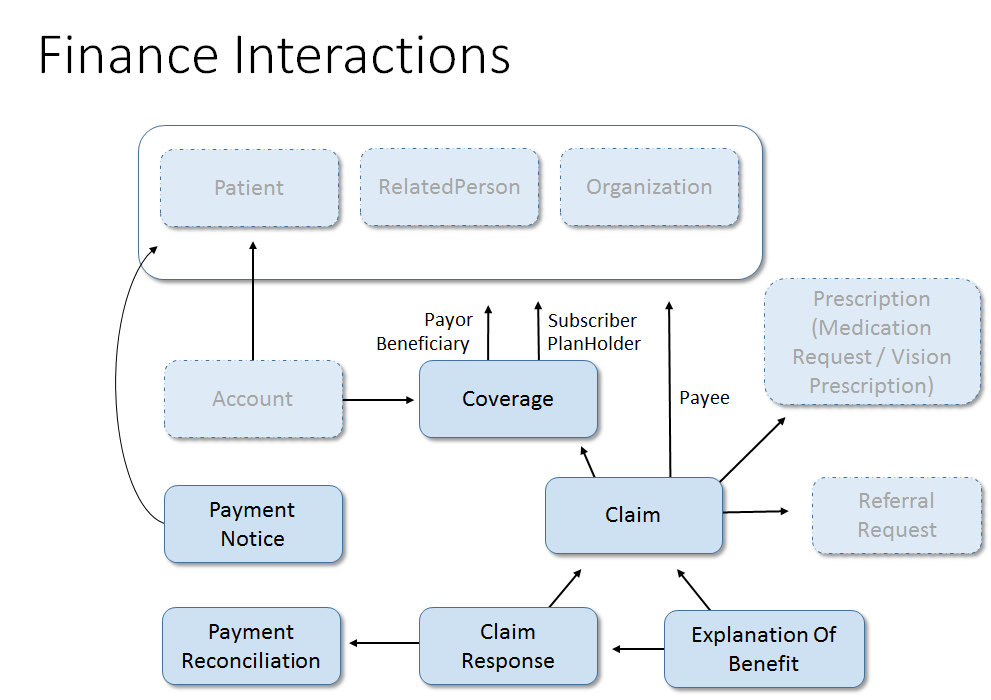
Image showing the relationship between the financial resources:
Additional Resources will be added in the future. A list of hypothesized resources can be found on the HL7 Confluence. Feel free to add any you think are missing or engage with one of the HL7 Work Groups to submit a proposal to define a resource of particular interest.
Financial information in general and in particular when related to or including health information, such as claims data, are typically considered Protected Health Information and as such must be afforded the same protection and safeguards as would be afforded to purely clinical identified health data.
The Security and Privacy measures associated with FHIR, such as the use of Security labels and tags in the resource.meta, are encouraged in addition to the use of whatever measures for authorization and encryption are supported by the chosen exchange model, e.g. FHIR REST, Web Services, Direct, MLLP, SMTP and others.
For more general considerations, see the Security and Privacy module.
The table below details various common business activities which occur in the financial realm, and the focal resources which may be exchanged, along with supporting resources, to accomplish the business activities. Whether the resources specified are actually needed requires consideration of the business itself and the exchange methodology and transport being used.
For example: If a content model is not required to obtain the appropriate status element then a SEARCH (GET) may be used, however if a content model is required to support the request for information then the content model will need to be CREATEd (POST). Alternately, if FHIR Operations are being used then the specified focal resource may be employed as one of the Operation parameters or might not be required.
| Business Activity | Request Resource | Response Resource |
|---|---|---|
| Eligibility Check | CoverageEligibilityRequest | CoverageEligibilityResponse |
| Enrollment Update | EnrollmentRequest | EnrollmentResponse |
| Claim | Claim (type={discipline}, use=claim) | ClaimResponse |
| Predetermination | Claim (type={discipline}, use=predetermination) | ClaimResponse |
| Preauthorization | Claim (type={discipline}, use=preauthorization) | ClaimResponse |
| Payment Notice | Task (code=deliver, input=PaymentNotice) | Task (output=error codes) |
| Payment Reconciliation | Task (code=poll, input=PaymentReconciliation) | Task (output=PaymentReconciliation) |
{discipline} means the type of claim: OralHealth, Vision, Pharmacy, Professional or Institutional.
See the Financial examples in Task for more details on Cancel, Nullify, Release, Reprocess, Status, and Poll operations.
Key financial terms and their definitions:
- Adjudication - The processing by an insurer of a claim, preauthorization or predetermination to determine under the insurance plan what if any benefits are or would be payable
- Beneficiary (Patient) - The party whose health care expenses may be covered by a policy issued by an Insurer
- Claim - A request to an Insurer to adjudicate the supplied charges for health care goods and services under the identified policy and to pay the determined Benefit amount, if any
- Coordination of Benefit (COB) - The rules, usually regionally defined, which govern the order of application of multiple Insurance coverages or Self-Pay to a given suite of health care expenses
- Insurer (Payer, Payor) - A public or private insurer which will adjudicate Claims for health care goods and services to determine if there is any benefit payable under the policy which covers the patient
- Policy - A contract between an Insurer and an individual or other entity such as an employer to reimburse covered parties (Beneficiaries) for some or all of a prescribed suite of health-related goods and services
- Preauthorization (Prior Authorization, Pre-Auth) - A request to an Insurer to adjudicate the supplied proposed future charges for health care goods and services under the identified policy and to approve the services and provide the expected benefit amounts and potentially to reserve funds to pay the benefits when Claims for the indicated services are later submitted
- Predetermination (Pre-Determination, PreD) - A request to an Insurer to adjudicate the supplied 'what if' charges for health care goods and services under the identified policy and report back what the Benefit payable would be had the services actually been provided
- Subscriber - The person who signs-up for the coverage. May be an employee or person with dependents
For the complete glossary, see the Financial Module documentation.
The table below details the relative order of events and use of financial resources for patient care during the care cycle. Not all steps or information exchanges may occur:
- Patient visits Provider
- Provider checks for valid insurance coverage (CoverageEligibilityRequest)
- Insurer responds with coverage status (CoverageEligibilityResponse)
- Provider examines Patient and reviews treatment options
- Provider submits Predetermination(s) for treatment options (Claim {use=predetermination})
- Insurer responds with potential reimbursement (ClaimResponse)
- Provider and Patient determine treatment plan
- Treatment plan submitted to Insurer to reserve funds (Claim {use=preauthorization})
- Provider provides treatment
- Provider submits patient's claim for reimbursement (Claim {use=claim})
- Insurer responds with claim adjudication (ClaimResponse)
- Patient leaves treatment setting
- Patient requests an Explanation of Benefit (ExplanationOfBenefit)
Resource Status Life-cycle: Financial resources begin with status 'draft' and continue with this status during development. When a resource is exchanged with an external party, the status changes to 'active'. An 'active' resource is immutable and cannot be edited except for status changes to 'cancel' or 'entered-in-error'.
Secondary Uses: In addition to their primary use of conveying patient billing information to insurers, many financial resources may be used to export data to other agencies to support reporting and analytics.
Attachments - Supporting Information: There is often a need to provide supporting information (attachments) to document the need for a service. This information may be provided inline in the resource's supportingInfo section, sent unsolicited in a Communication, or sent in response to a CommunicationRequest.
Subrogation: In some cases, it's not appropriate to send Claims to certain insurers due to jurisdictional rules. The Coverage resource supports marking coverages as subrogation to handle downstream recovery of costs.
Coordination of Benefit (COB): When a patient has multiple Coverages, there will be an agreed order of application of claims recovery. Claims work through the COB order until exhausted or no further balance remains.
Batches: eClaims request and response resources may be exchanged individually or via batches using Bundle resources.
Real-time Exchange: The eClaims resources are intended to support real-time exchange, though in many cases responses will only indicate receipt and validation, with deferred responses obtained later via REST or Poll operations.
The Financial Management Work Group (FM) is responsible for two subdomains:
- Financial Accounts and Billing (FIAB) - resources for accounts, charges (internal costing transactions) and patient billing
- Financial Claims and Reimbursement (FICR) - insurance information, enrollment, eligibility, predetermination, preauthorization, claims, patient reporting and payments
To date FM has been focusing on the resources required to support the exchange of claims and related information between health care providers and insurers. The first draft of this work is nearing completion with the first Financial Standard for Trial Use. Over the next year further refinements are expected as implementers begin developing regional profiles and begin live pilots with resources.
Once the above is well underway FM can then look to developing the Enrollment-related resources and the resources to support the FIAB functions.
In many cases an example valueset has been provided in this release. Financial Management will be devoting effort in the preparation to Release 5 of FHIR to develop more representative example sets and to determine where global codesets exist such that some of the valuesets may be elevated in strength to extensible or required.
https://docs.heydonto.com/_mock/apis/fhir/financial/
https://api-staging.heydonto.com/
https://api.heydonto.com/